
In the Heat of the Olympics
As a result of the high metabolic heat production and heat gain by physical contact with the surroundings, exercising in the heat poses a formidable challenge to the body’s ability to regulate its internal environment. Increased sweating onto the skin is induced as a way to limit the increase in core temperature. Generally, restricting core temperature and extending the time before reaching a limiting temperature will result in body water and electrolytes losses. In some cases, the reduction in blood volume is partially offset by cardiopulmonary adaptations, such as increased heart rate and peripheral resistance, but they are not sufficient to maintain function. Long-term prolonged exercise and short-term high-intensity exercise will both be impaired by dehydration. Due to inadequate replacement of fluid losses, athletes who train and live in the heat could suffer from chronic Hypohydration. By drinking water or other appropriate fluids, the adverse effects of exercise in the heat are minimized. Hydration strategies should be tailored to the athlete’s exercise task, environmental conditions, and individual physiological characteristics. There may also be an advantage to manipulating pre-exercise body temperature, especially when competing in stressful environments.
The effects of heat on exercise
It is generally accepted that exercising in the heat impairs endurance performance even though most athletes prefer warm climates for training and competing. There is some reduction in exercise capacity even at modest environmental temperatures, and the reduction becomes progressively more significant as environmental temperatures rise (Galloway and Maughan, 1997; Parkin et al., 1999). At least in the laboratory, the optimum temperature for endurance performance is about 10C, which raises the question of whether particular strategies are required when the ambient temperature exceeds this threshold. Performance is reduced in the heat partly because of progressive dehydration, adversely affecting cardiovascular capacity and thermoregulation (Gonzalez Alonso et al., 1999a). Hypohydration also affects metabolic function and exercise performance more intensely in hot weather than in cold weather (Coyle, 2004). Thus, Hypohydration, which is tolerable in cool or temperate weather conditions, can interfere with performance in hot weather conditions. A difference between heat and cold may be related to fatigue of the central nervous system (CNS), and the CNS may more influence that performance impairment in the heat than by the muscles (Nielsen et al., 2001; Nielsen and Nybo, 2003). There has been mixed success in manipulating the CNS component of fatigue: Although pharmacological interventions involving prohibited drugs have been shown to alter performance, nutritional manipulations affecting neurotransmitter synthesis have been less successful (Davis et al., 2000).

As a result of COVID-19, the 2020 Tokyo Olympics have been postponed by one year to 23 July to 8 August 2021. Despite this delay, the Olympics will still be held in the summer in one of the world’s busiest and most humid cities. In the years leading up to the original 2020 Olympics, temperatures reached 41C, with over 65 heat-related deaths recorded in a single week. A group of experts created by the International Olympic Committee (IOC) implemented various countermeasures and developed educational materials for athletes, workers, and spectators in response to this concern. It appears, however, that the translation of research into practice varies considerably across nations, sports and athletes, despite the abundant scientific literature describing training in the heat.
This issue extends far beyond Tokyo 2020, as Paris (2024) is frequently plagued with heat waves during the Olympic period, and the best world record temperature was recorded in California (*200 miles from Los Angeles 2028).
The purpose of this article is to provide a deeper understanding of the problem (i.e., Epidemiology and environmental conditions), athlete calendar planning (i.e., Traveling to acclimate vs. traveling to compete), on-site countermeasures (Hydration and Cooling) and, in case those preventive measures fail, the evidence-based management of the exertional heat-stroke (Prevention and treatment of EHS). The brief evidence-based summaries included in all sections will assist busy clinicians and practitioners.
Epidemiology and environmental conditions
During heat-exertion, athletes’ core temperatures can reach above 41°C (Racinais et al., 2019). Most of the information includes special considerations for Football (Nybo et al. 2020) and an analysis of 8530 elite beach volleyball matches (Racinais et al. 2000), revealing the risks associated with playing in the heat when not accustomed to it. In addition, the editorial from Notley et al. (2020) (which features the figure below) challenges the notion that men and women have different thermoregulatory strategies, as all humans are challenged by acute heat exposure but can adapt regardless of gender.
Despite the definition of “heat” and evaluating heat stress being relatively well established, there is still some discussion regarding the factors contributing to heat stress, including temperature, humidity, radiation, and airflow. Grundstein and Vanos (2020) explain the complexity in their editorial, and Thorson et al. (2020) provide original data challenging the traditional WBGT used by most International Federations (IFs).
This video by Professor Sebastien Racinais on the environmental temperature and elite athletes is another highly recommended summary of the issue.
Traveling to acclimate vs. traveling to compete
To compete in heat adaptation, countermeasures must be taken (Racinais et al., 2015). However, while 61% of elite cyclists responding to the questionnaire described prior exposure to heat before a world championship, only 38% were reported to have an acclimation protocol in place (Racinais et al. 2020).
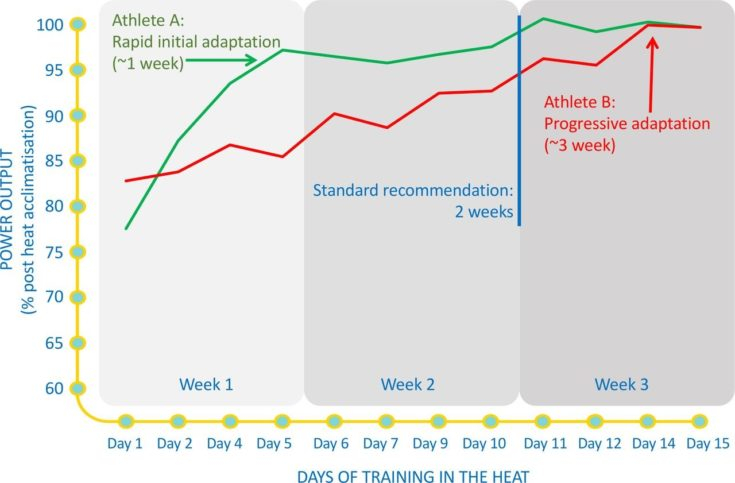
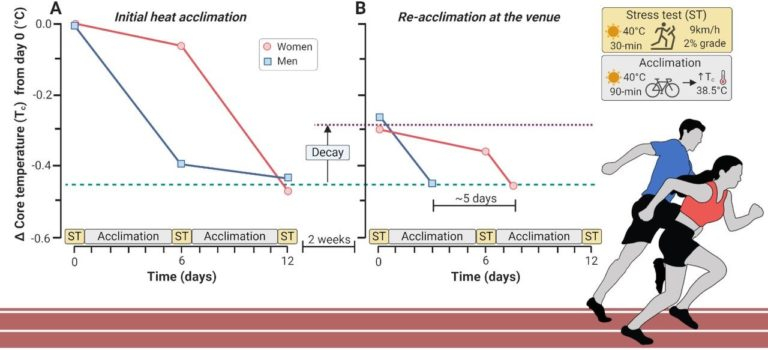
An illustrated figure (below) shows how heat acclimation can be personalized (Racinais and Ihsan 2020), as well as recovery options (Ihsan et al. 2020), as well as how to schedule them (Racinais and Periard 2020).

Hydration and Cooling
The tapering period should be acclimatized in advance to avoid a last-minute physiological and perceptual load (Racinais and Periard 2020), as shown in this figure.

Athletes should focus on their hydration (Periard et al. 2020) and cooling (Bongers et al. 2020) on race day, which should have been tested beforehand (Taylor et al. 2020). Anecdotally, similar cooling techniques are also employed to alleviate the effects of COVID-19-induced heat stress on personal protective equipment (PPE) (Bongers et al. 2020).
Prevention and treatment of EHS
Imagine that despite all these precautions, an athlete is suffering from exertional heat stroke (EHS). The IFs need clear policies and procedures in this case (Mountjoy et al. 2020), including an adequate emergency plan, adapting the rules, and educating and training athletes (Parsons et al. 2020). In addition, the local organizing committee should implement a ‘heat-deck’ to facilitate rapid on-site cooling, according to (Hosokawa et al. 2020). Other issues presented in this section include heat stress during pregnancy (Ravanelli 2018) or digestive disorders (Snipe 2018).
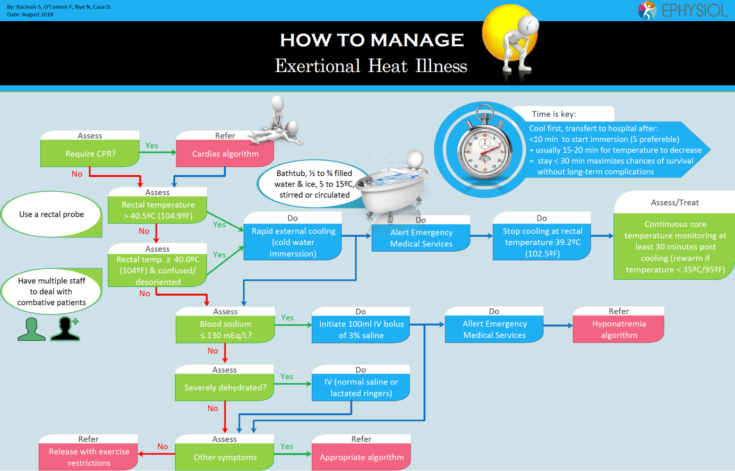
To listen to a great talk about what organizations and events need to consider and implement in order to mitigate heat risks for both athletes and spectators for the upcoming Olympic Games, click on this link. Presenters are members of the IOC Working Group planning for the Tokyo 2020 Games, Sebastien Racinais (Aspetar, Qatar) discusses the progression of event management at major games, Doug Casa (Korey Stringer Institute, USA) gives a historical and evidence-based talk on the treatment of exertional heat stroke (EHS) and Yuri Hosokawa (Waseda U, Japan) provides detailed insight on her working with Tokyo 2020 on EHS planning.
References:
1. Bongers CC, de Korte JQ, Catoire M, et alInfographic. Cooling strategies to attenuate PPE-induced heat strain during the COVID-19 pandemic. British Journal of Sports Medicine 2021;55:69-70.
2. Bongers CCWG, de Korte JQ, Eijsvogels TInfographic. Keep it cool and beat the heat: cooling strategies for exercise in hot and humid conditions. British Journal of Sports Medicine 2021;55:643-644.
3. Coyle, E.F. (2004). Fluid and fuel intake during exercise. Journal of Sports Sciences, 22, 39–55.
4. Davis, J.M., Alderson, N.L. and Welsh, R.S. (2000). Serotonin and central nervous system fatigue: nutritional considerations. American Journal of Clinical Nutrition, 72, 573S–578S.
5. Galloway, S.D.R. and Maughan, R.J. (1997). Effects of ambient temperature on the capacity to perform prolonged cycle exercise in man. Medicine and Science in Sports and Exercise, 29, 1240–1249.
6. Gonzalez Alonso, J., Calbet, J.A. and Nielsen, B. (1999a). Metabolic and thermodynamic responses to dehydration-induced reductions in muscle blood flow in exercising humans. Journal of Physiology, 520, 577–589.
7. Hosokawa Y, Casa DJ, Racinais STranslating evidence-based practice to clinical practice in Tokyo 2020: how to diagnose and manage exertional heat stroke. British Journal of Sports Medicine 2020;54:883-884.
8. Ihsan M, D. Périard J, Racinais SHow to integrate recovery during heat acclimation. British Journal of Sports Medicine 2021;55:185-186.
9. Mountjoy M, Moran J, Ahmed H, et alAthlete health and safety at large sporting events: the development of consensus-driven guidelines. British Journal of Sports Medicine 2021;55:191-197.
10. Nielsen, B., Hyldig, T., Bidstrup, F., Gonzalez-Alonso, J. and Christoffersen, G. (2001). Brain activity and fatigue during prolonged exercise in the heat. Pflugers Archive, 442, 41–48.
11. Nielsen, B. and Nybo, L. (2003). Cerebral changes during exercise in the heat. Sports Medicine, 33, 1–11.
12. Nybo L, Flouris AD, Racinais S, et alFootball facing a future with global warming: perspectives for players health and performance. British Journal of Sports Medicine 2021;55:297-298.
13. Notley SR, Racinais S, Kenny GPDo sex differences in thermoregulation pose a concern for female athletes preparing for the Tokyo Olympics? British Journal of Sports Medicine 2021;55:298-299.
14. Parsons JT, Anderson SA, Casa DJ, et alPreventing catastrophic injury and death in collegiate athletes: inter-association recommendations endorsed by 13 medical and sports medicine organizations. British Journal of Sports Medicine 2020;54:208-215.
15. Périard JD, Eijsvogels T, Daanen HAM, et alHydration for the Tokyo Olympics: to thirst or not to thirst?British Journal of Sports Medicine 2021;55:410-411.
16. Racinais S, Moussay S, Nichols D, et alCore temperature up to 41.5ºC during the UCI Road Cycling World Championships in the heat. British Journal of Sports Medicine 2019;53:426-429.
17. Racinais S, Alhammoud M, Nasir N, et alEpidemiology and risk factors for heat illness: 11 years of Heat Stress Monitoring Programme data from the FIVB Beach Volleyball World Tour. British Journal of Sports Medicine Published Online First: 12 October 2020. doi: 10.1136/bjsports-2020-103048
18. Racinais S, Nichols D, Travers G, et alHealth status, heat preparation strategies and medical events among elite cyclists who competed in the heat at the 2016 UCI Road World Cycling Championships in Qatar. British Journal of Sports Medicine 2020;54:1003-1007.
19. Racinais S, Ihsan M Why should I test my athletes in the heat several months before Tokyo 2020? British Journal of Sports Medicine 2020;54:700-701.
20. Racinais S, Périard JDBenefits of heat re-acclimation in the lead-up to the Tokyo Olympics. British Journal of Sports Medicine 2020;54:945-946.
21. Ravanelli N, Casasola W, English T, et alHeat stress and fetal risk. Environmental limits for exercise and passive heat stress during pregnancy: a systematic review with best evidence synthesis. British Journal of Sports Medicine 2019;53:799-805.
22. Racinais S, Alonso JM, Coutts AJ, et alConsensus recommendations on training and competing in the heat. British Journal of Sports Medicine 2015;49:1164-1173.
23. Snipe RMJExertional heat stress-induced gastrointestinal perturbations: prevention and management strategies. British Journal of Sports Medicine 2019;53:1312-1313.
24. Taylor L, Carter S, Stellingwerff T. Cooling at Tokyo 2020: the why and how for endurance and team sport athletes. British Journal of Sports Medicine 2020;54:1243-1245.
25. Vanos JK, Grundstein AJ. Variations in Athlete Heat-Loss Potential Between Hot-Dry and Warm-Humid Environments at Equivalent Wet-Bulb Globe Temperature Thresholds. J Athl Train. 2020 Nov 1;55(11):1190-1198. doi: 10.4085/1062-6050-313-19. PMID: 33112954; PMCID: PMC7709211.
26. Posters and guidance used from the Special BJSM e-Edition on #OlympicsInTheHeat.

